Ortho for the USMLE: Identifying Pediatric Non-Accidental Trauma
- by
- Nov 20, 2018
- Reviewed by: Amy Rontal, MD
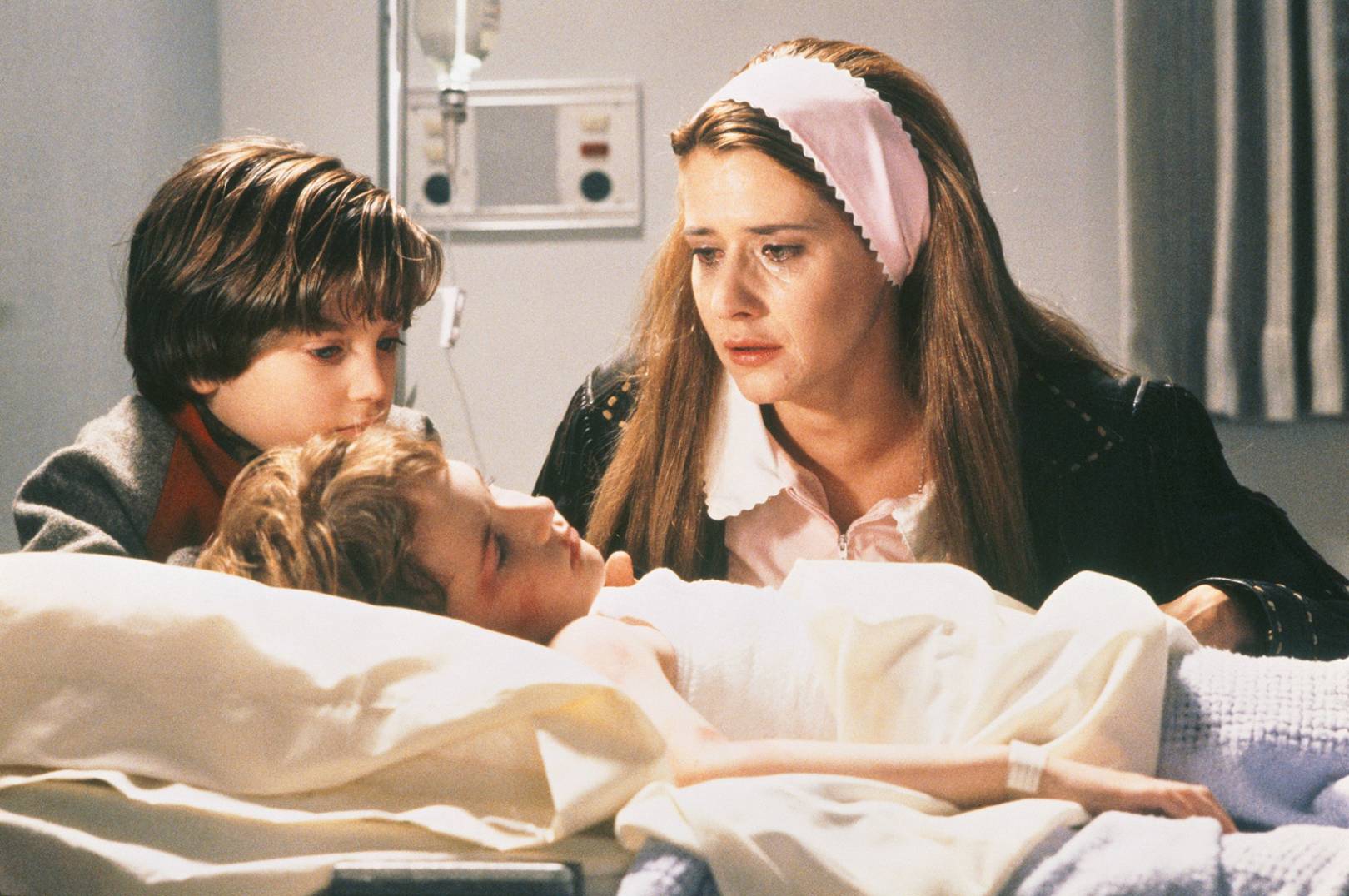
Pediatric non-accidental trauma (child abuse) can be one of the most emotional and stressful diagnoses to work up. Your job as the physician is (1) to recognize the potential for non-accidental trauma, (2) bring the patient into the hospital for safe evaluation, (3) provide an objective assessment of the injury pattern, (4) treat the injuries, and (5) notify the appropriate authorities who can ensure the patient’s safety upon discharge.
Recognizing non-accidental trauma can be difficult, but is very important. Unrecognized or unreported child abuse portends up to 50% chance of repeat abuse and up to 10% risk of mortality from subsequent abuse. Risk factors to look for in the child include a child of an unplanned pregnancy, premature children, children with disabilities, and children of divorced parents or those with step parents. Risk factors for the parents include those in a single-parent home, those affected by a socioeconomic stressor think recent move, job change, unemployment, lower socioeconomic status, or lack of a support system those with a history of illicit drug use, or those with a personal history of abuse. The USMLE may give you these clues or just blatantly state that child abuse is suspected. Regardless, children with injuries and these risk factors must be admitted to the hospital for further workup. The conversation with the parent or caregivers should not admit to concern for non-accidental trauma. Rather, you should state that this workup is routine, that further tests or x-rays may be taken, and that they may meet with multiple other physicians and health care providers depending upon the outcome of those tests. You also may need to remove distant or dangerous individuals from the situation to safely explain this next step. Your goal is to take care of the child safely, while maintaining a trusting relationship with the parents or caregivers.
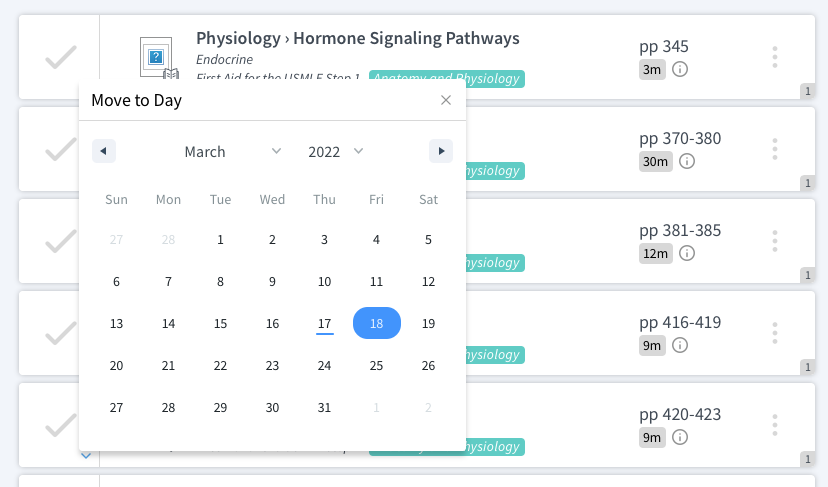
Distinguishing non-accidental trauma from normal injury starts with a good history and physical examination. In conjunction with the risk factors we just discussed, a history of delay in seeking care, inconsistent history from the caregivers, or time away from the primary caregiver should raise your suspicion. The injury pattern should also match the history. Any injury that the patient cannot inflict on themselves should raise your suspicion for non-accidental trauma. Think fractures of the ribs, scapula, sternum, and spinous processes, complex skull fractures, retinal hemorrhages, multiple bruises, burns, lower extremity fractures in patients who cannot yet ambulate or injuries in various stages of healing. To look for these, pediatric patients with suspected non-accidental trauma will undergo a skeletal survey (radiographs of every bone in the body), CT scan of the head, and ophthalmologic examination so that the appropriate consultants can be notified and treatment initiated.
Back to orthopaedics. Long bone fractures in a nonambulator should always raise concern for non-accidental trauma. There is no way that a healthy infant without metabolic derangements can break his femur. However, an ambulatory toddler or young child may easily sustain a spiral fracture in the femur or tibia from a plant and twist mechanism. So just because you see a spiral fracture does not mean you are dealing with child abuse. A spiral injury simply represents a low energy pattern of twisting. In the athlete, a twisting injury of the ankle may result in ankle sprain and a twisting injury in the knee may result in an ACL rupture; twisting injury in the overweight individual may cause ankle fracture or tibial plateau fracture; and in the young child, planting the foot and twisting may result in a spiral femur or tibia fracture, the latter known as a toddler’s fracture. So, if the patient can ambulate and presents with a spiral fracture, it does not necessarily rule in non-accidental trauma. However, the converse is true. Nonambulatory children, toddlers and infants should never have lower extremity fractures, because they cannot twist on their own. It requires an external force to do so.
Remember, it is possible that the patient has a metabolic abnormality such as osteogenesis imperfecta, osteopenia of prematurity, scurvy, or chronic renal or liver disease that is producing weak bones, skin, or blood vessels prone to injury that must also be elucidated as a potential etiology of injury.
If you think you see child abuse, take the appropriate steps to admit the patient to the hospital for safe workup and treatment. You will not be faulted for admitting a child with a truly accidental injury. Injuries you should look out for include any injury that the child cannot inflict on themselves such as long bone injuries in a nonambulatory patient, rib fractures, scapula fractures, spine fractures, complex skull fractures, multiple injuries, and injuries in various stages of healing. Safety comes first. On the USMLE, if non-accidental trauma is suspected, pick the answer that provides expeditious and thorough care to the patient in a hospital setting, while also maintaining a trusting relationship with a distraught and heartbroken family.