Mastering Mnemonics for the USMLE: AEIOU Isn’t Just for Learning Grammar
- by
- Apr 07, 2021
- Reviewed by: Amy Rontal, MD
Dr. Christopher Carrubba, Dr. Brian Radvansky, and Dr. Taylor Purvis contributed to this article.
“Why is our patient on dialysis?” If I had a dollar for every medical student that asked me this question, I could definitely afford a nice meal out with my wife. I’ve found that many students have a minimal understanding of dialysis and think that its only usage is in the care of patients with chronic kidney disease—I know I certainly did once upon a time.
Unfortunately, that limited understanding can come back to bite you on Step 2 when you are often required to know if a patient is a dialysis candidate. Moreover, understanding the uses of dialysis is a surefire way to impress your team on a medicine wards month or a nephrology rotation. We’ll also spend some time at the end of the article addressing what “dialysis” really means, so that you can sound extra-impressive on the wards.
As always, we’re here with mnemonics to make it easy!
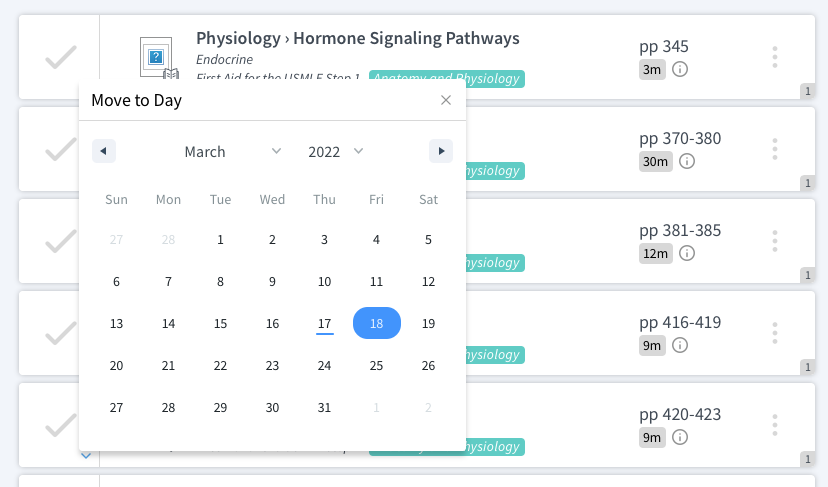
AEIOU Mnemonic: Indications for [Emergent] Dialysis
For this mnemonic, each letter corresponds to a specific indication for dialysis. As with many mnemonics, some creative liberties were definitely taken to make everything line up. Let’s see how it breaks down.
A = acidosis
More specifically, severe metabolic acidosis. Now don’t go rushing to put everyone with metabolic acidosis on dialysis. Just remember that this is an option for very severe and refractory cases.
In some situations, a patient’s metabolic acidosis will be wreaking havoc on the milieu of their blood and body’s enzymes. Our bodies weren’t designed to run at pH 6.9. Pressors/inotropes won’t work as well, myocytes will be depressed. There will be [necessary] hyperventilation. Take, for instance, a patient with a sky-high lactate from cardiac arrest, who has developed shock liver from the period of hypotension. Their busted liver will be unable to clear the lactate, and their only hope to do so (other than restoration of perfusion and heart function), will be dialyzing it off.
E = electrolyte abnormalities
Most commonly, hyperkalemia. For patients with severe hyperkalemia (i.e. bad enough to cause peaked T waves and a widening QRS on an EKG) +/- poorly functioning kidneys, dialysis is an excellent and sometimes necessary option to remove the potassium. However, if the patient’s kidneys are functioning properly, always consider other options first.
Remember your hyperkalemia protocol: start with insulin to drive that K+ into cells (and glucose/dextrose if the insulin will lead to hypoglycemia). Administer calcium to stabilize cardiac myocytes and prevent malignant arrhythmias. Furosemide (lasix) can also help send some K+ out of the body, and fits nicely into the schema.
If you have a true hyperkalemic emergency, dialysis is your last resort.
I = intoxication
This is probably the least common usage of dialysis these days; but it remains an option for lithium toxicity, TCA overdose, and alcohol intoxication. Nasty chemicals in the blood causing problems? Dialyze them out.
O = (volume) overload
For patients suffering from volume overload secondary to chronic (or even acute) kidney disease, this is a very common reason for dialysis. If your kidneys are not able to make urine, you don’t have an exit strategy for the fluids that enter your body. Many ICU patients are on loads of IV infusions, and if they can’t pee out all that fluid, it’s going to end up in interstitial spaces where it doesn’t belong.
How bad does volume overload have to get? Puffiness itself won’t kill your patient. But pulmonary edema and increasing oxygen requirements might.
U = uremia
In terms of the USMLE, this is probably the most tested indication for dialysis. For patients with chronic kidney disease complicated by uremic pericarditis or encephalopathy, dialysis can be a life saving intervention.
There is no hard and fast cutoff for dialyzing at a certain BUN (blood UREA nitrogen). But if the patient suffers from pericarditis, refractory nausea/vomiting, or encephalopathy, dialysis is indicated.
Initiating dialysis is no small feat; it’s not a simple box to check. Patients who require dialysis require dialysis ACCESS. If they were on dialysis as outpatients, they probably have some established access like a AV graft or fistula. But if there’s an acute indication in a dialysis-naive patient, they will have to get an extra large central line placed, in order to support the flows necessary to send blood to-and-from the dialysis machine. So before you start placing giant lines in central veins, make sure that the patient has a necessary indication, and that it cannot be handled (timely) with a non-invasive intervention.
What You Need to Know About Dialysis
Before we let you go, we want to break down what “dialysis” really means. Technically, this article was referring in general to “renal replacement therapy.” You’re supporting the kidneys in their time of need with a form of replacement therapy. There are actually multiple modalities of replacement therapy. We won’t get into too much nitty-gritty, but it’s helpful to know the big differences.
These modalities of renal replacement therapy are:
- Intermittent hemodialysis
- Continuous renal replacement therapy
- Hybrid therapies like sustained low-efficiency dialysis (SLED)
- Peritoneal dialysis
Intermittent hemodialysis (IHD) is, well, intermittent. Think 3-4 hours, 3 times a week type of thing. This is probably the one you think of the most in your ambulatory CKD patients who go to an outpatient dialysis center. It can be used in emergent cases too, though. These are big fluid shifts over a short period of time, though, and can cause cardiovascular instability.
Continuous renal replacement therapy (CRRT) is commonly used in critically ill patients. It’s what it sounds like: a continuous, 24-hours-a-day filtration. It has great hemodynamic stability because you’re clearing things slowly over the course of the day.
Hybrid therapies like SLED are sort of the goldilocks in between IHD and CRRT. SLED, for example, is done 6-12 hours a day with pretty good hemodynamic stability. This can be used in critically ill patients or in treating things like hyperkalemia.
Peritoneal dialysis is rarely used for acute therapy in the US, though it technically can be. A catheter is surgically placed into the peritoneal cavity rather than in the vasculature.
We hope this helps clear up some of the confusion about “dialysis”! Now you know how to write accurately about your patients in the hospital who are undergoing renal replacement therapy.
Good luck out there!