Mechanical Ventilation Algorithm for Rotations and USMLE Questions
- by
- Jun 08, 2021
- Reviewed by: Amy Rontal, MD
In our recent Acute Respiratory Distress Syndrome (ARDS) and Mechanical Ventilation webinar, we covered a lot of ground:
- Basics of ARDS and mechanical ventilation
- Respiratory physiology review
- Indications, mechanism & ventilation parameters
- Arterial blood gas analysis interpretation
- Interventions and management of abnormal ABGs
- Diagnosis, management, and more
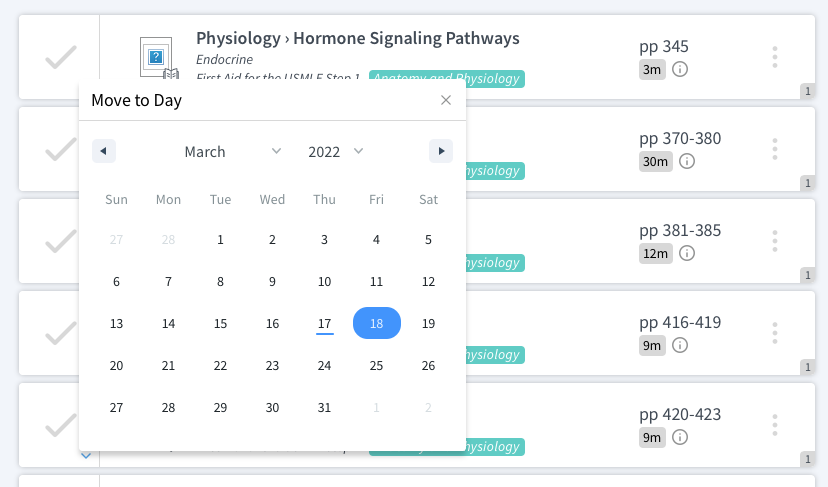
In particular, we went over an algorithm that covers the four key variables of mechanical ventilation. You’ll need to know this for your rotations and questions you’ll encounter on the USMLE and COMLEX.
Below, we’ve included the transcript for the five minutes or so that we discussed the algorithm, and you can also check out the full webinar, which is included at the bottom of this post.
4 Key Variables for Mechanical Ventilation Questions on the USMLE & COMLEX
Really good question asked by a student here: How do we interpret the PaO2 value?
So, the oxygen levels obviously vary quite a lot in patients — which you know from your own experience with questions or patients where oxygen saturation is 92% in this patient, 96% in this patient. Saturation correlates with PaO2 value, even if they’re not exactly the same.
And so what that means is that there’s a variety of numbers that we might be okay with when it comes to PaO2. But the general rule of thumb that I would stick to is that if someone has a PaO2 value that’s falling lower than 70 on the exam — so, 70mm of mercury, the normal value being 100 in a normal, healthy individual — if it falls below 70, we start to kick in what’s called our hypoxic drive.
So what I want to emphasize here is that all of us have a respiratory driver that’s telling our medulla how fast we should be breathing. Before I mentioned it, you all were probably breathing autonomously — now you’re all probably thinking about breathing at this point. Sorry about that. But before that, you were breathing at a certain rate based on the CO2 level in your blood.
Everybody at baseline is operating on what’s called a hypercapnic drive. We keep CO2 exactly at 40. If it goes a little above 40, we start to hypoventilate a little to bring things down. If we breathe a little too fast and the CO2 goes down, our brain stem tells us to stop breathing so much so we can help bring it back up to 40.
40 is THE number that we’re seeking for PaCO2.
As a result, we’re going to be laser-focused on that. But what if oxygen levels drop despite the fact that our CO2 is okay?
If that happens, now we’re going to start breathing faster for oxygen. We’re not very good at that. The hypoxic drive doesn’t really improve our oxygen very well. Imagine yourself going up to the top of a tall mountain where the environmental oxygen is 60 mm of mercury, you’ll breathe very fast because you’re hypoxic, but you won’t really fix your oxygen level as a result.
So our hypoxic drive is another way that we’ll breathe fast. But the reason I’m bringing up our respiratory drivers is because CO2 and O2 are the two things we’re paying attention to when we intubate a patient.
How to Answer Mechanical Ventilation Questions on Rotations and USMLE Exams:
When you are asked a question on mechanical ventilation and they say, “What do you want to do? How do you fix this patient who’s being intubated and mechanically ventilated?”
In the vast majority of cases, they’re going to be asking you:
• Should I be fixing the oxygen: yes or no?
• Should I be fixing the carbon dioxide: yes or no?
• And how would I fix the carbon dioxide or the oxygen in this patient?
And so if the CO2 value is not 40, you probably want to fix it. If the oxygen value is below 70, that’s probably where you need to start making an intervention for that patient.
For reference, somewhere around 60 mm of mercury is roughly around 88% oxygen saturation, and that’s the number clinically that we really hate to go below, around 88–89%, in that territory.
So when the oxygen falls below 70, or in the 60s, or below that, that’s where we’re going to want to intervene. And that comes to: How do we intervene?
Now, for oxygen, the first answer is super easy: just give the patient more oxygen. So the fraction of inspired oxygen, super straightforward answer: just give them some more of that. That should improve their oxygenation in the majority of cases.
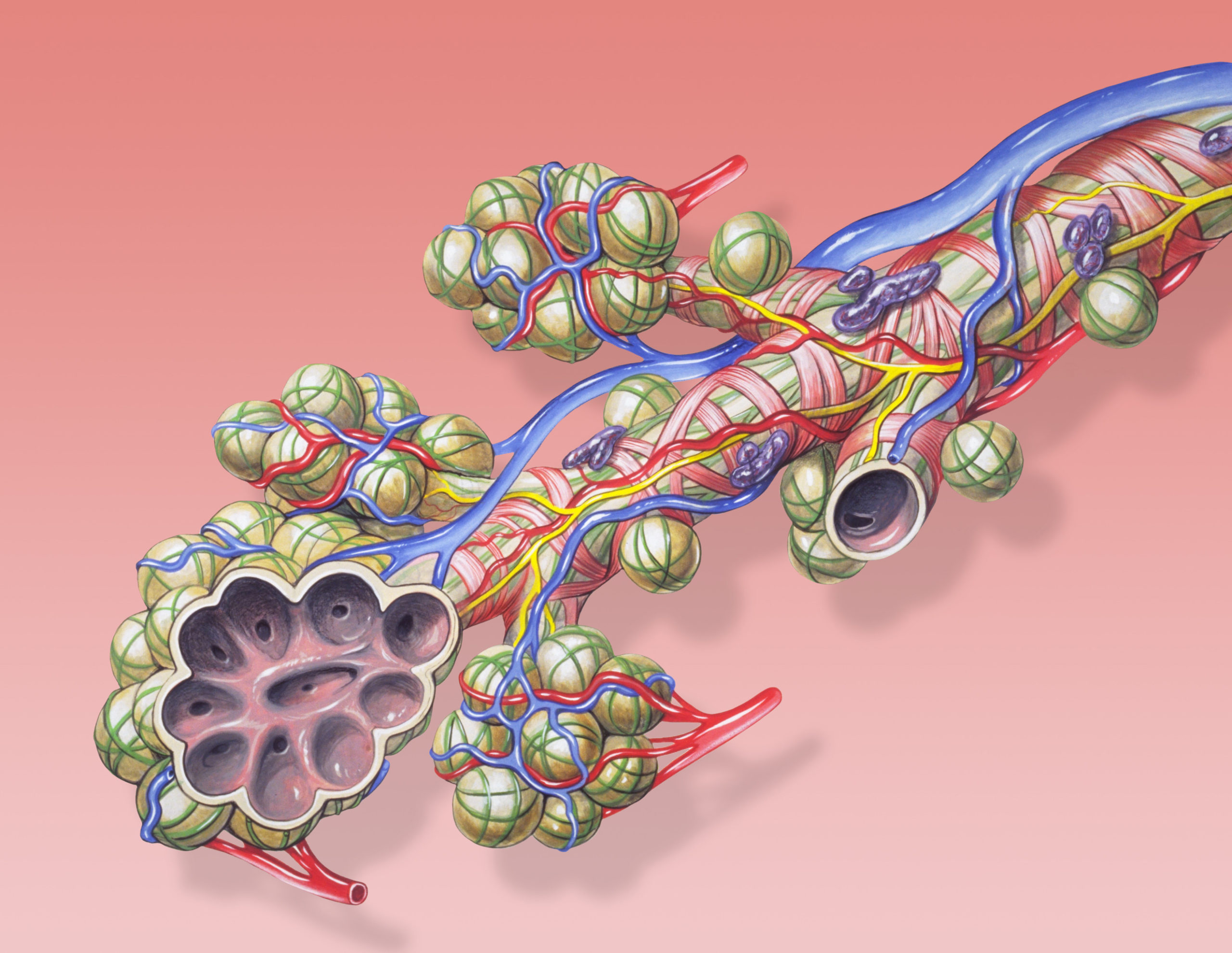
The other way that we can fix oxygen is called PEEP — or, positive end-expiratory pressure. I’m going to set that aside for a second. We’ll come back to defining what that means in a second.
And for carbon dioxide: the real thing that matters for CO2 is the respiratory rate and the tidal volume. These two values roughly equate to what’s called minute ventilation.
Minute ventilation is like the cardiac output but for your lungs.
Respiratory Rate x Tidal Volume = how much air your lungs are moving around, essentially.
And because CO2 is not a diffusion-limited gas in the way that oxygen is, I really don’t care what’s happening to the lungs. As long as I’m moving air, I’m probably breathing out CO2 in these cases.
There’s a direct correlation, an inverse relationship: The more you’re breathing, the less CO2 we’ll have.
And so that means, if you want your patient to have less CO2, you increase their respiratory rate or you increase their tidal volume. If you want them to have more CO2, you decrease their respiratory rate or you decrease their tidal volume.
So, CO2 is a little more tricky than oxygen insofar as it can be high or low, and you want to fix it. Oxygen generally just goes low and you want to bring it back up.
These are the only four variables that you’re ever really going to choose in questions about mechanical ventilation.
You’re going to see repetitive questions on UWorld, on NBME practice tests, and on the real exam — they’re just going to be asking the same thing over and over again.
And so, when we start equipping ourselves with knowledge that we can only really answer these four things for mechanical ventilation questions, they become a lot easier to understand.
Anything to add to that, Sana?
I really love the way you outlined the differences. This should be an algorithm for all of you:
When you see a mechanically ventilated patient, and they’re asking “What do we do now?” It’s always going to be: Which one’s wrong? And then, if so, one of these things is already going to be optimized, and one of them is not.
Working your way down that algorithm is going to answer 99% of the mechanical ventilation questions you’re going to see.
Watch our full ARDS & Mechanical Ventilation Webinar: