A Guide to Shock and the Cardiovascular System for the USMLE
- by
- Sep 09, 2020
- Reviewed by: Amy Rontal, MD

If you had to reduce the function of your cardiovascular system to one goal, how would you describe it? What is the primary purpose of the heart and blood and vasculature?
At the center of it all is the need to deliver oxygen to the organs and tissues of the body. Sure, there is some element of carrying away wastes and delivery of nutrients, but central to it all is oxygen delivery.
How is said oxygen delivered? Quite simply, blood has the ability to carry oxygen, and the heart pumps this oxygen-laden blood to the organs that so desperately need it.
An often forgotten but essential medical physiology equation is the one that governs delivery of oxygen (DO2):
Delivery of oxygen = Cardiac Output x Arterial Oxygen content
DO2 = CO x CaO2
A further derivation of oxygen content gives us the equation:
CaO2 = (1.39 x Hb x SaO2) + (0.003 x PaO2)
Where Hb = hemoglobin, SaO2 = oxygen saturation, and PaO2 = partial pressure of dissolved oxygen in arterial blood.
The second part of the above equation (0.003 x PaO2) is not very significant unless very high FiO2 is used, or in cases of severe anemia. Assuming an off-the-charts PaO2 of 500, and much more down-to-earth values for Hb (10) and SaO2 (100%), our two terms would be 13.9 and 1.5 respectively; the second pales in comparison to the first.
Summing it all up, in order to get oxygen to the tissues, you need:
- Cardiac Output (which depends on pre-load, afterload, and contractility)
- Hemoglobin
- Oxygen saturating this hemoglobin
If any one of these suffers, you’ve got a patient who might be headed towards, or already in shock.
Now that we’ve laid the physiologic groundwork, let’s apply it clinically to some scenarios you might see on a USMLE exam.
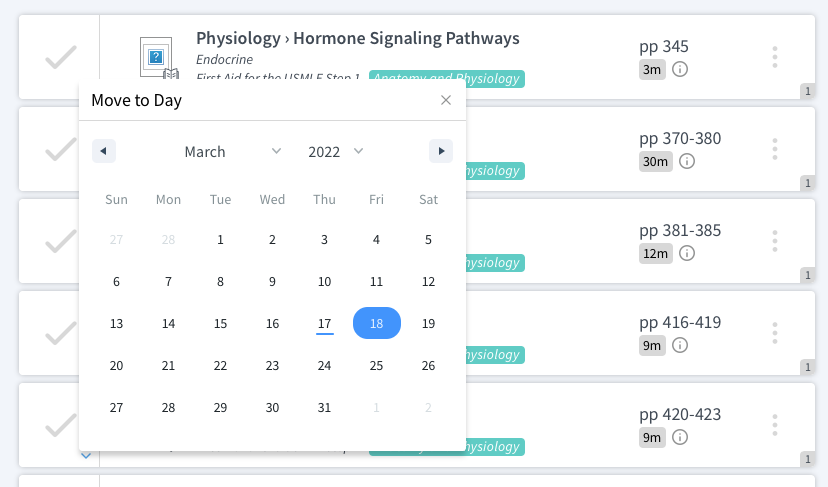
Shock Scenarios on the USMLE Exam
Most shock states will be due to decreases in cardiac output, which must come from a disruption in preload or contractility. Enormous afterload might decrease forward flow, but more often than not, shock stems from an empty tank, a body whose tank acts as though it were empty, or a pump that is not doing its job.
Hypovolemic Shock
Hypovolemic shock is probably the easiest to comprehend. A patient presents with intravascular depletion for one reason or another (e.g., hemorrhage, GI losses), and there’s not enough fluid or hematocrit in the vasculature to maintain a blood pressure, or to deliver oxygen to needy tissues.
Signs include decreased filling pressures (low CVP, low PCWP) and a high SVR as the body tries to compensate for an empty tank. Treatment is simple: give blood and IV fluid!
Cardiogenic Shock
Cardiogenic shock is also quite straightforward. A busted pump fails to generate the “oomph” necessary to propel blood and oxygen to the tissues that need it. In our DO2 = CO x CaO2 equation above, we have lost the CO aspect. Causes here include acute MI, chronic heart failure, or valvular abnormalities that impede forward flow.
Signs include high or low filling pressures (high if a busted LV causes a backup of sorts, and low if right heart failure is preventing the left side from filling), and increased SVR. Treat with inotropes to whip the tired heart and promote some degree of forward flow and oxygen delivery.
Obstructive Shock
Obstructive shock lives up to its name. There is physical obstruction that prevents the heart from doing what it needs to do. This obstruction can make preload plummet when it occurs in the vasculature; public enemy number one is a pulmonary embolism. Obstruction can also occur from extra-cardiac sources like a tension pneumothorax or cardiac tamponade. As above, depending on the cause of obstruction, filling pressures can be high or low. SVR will be elevated to try to create some blood pressure in the setting of low output. Treat the cause and relieve the obstruction, using pressors and fluids to temporize.
Distributive Shock
Distributive shock is the oddball of the bunch. Your main players here are anaphylaxis/sepsis and spinal shock. The hallmark of anaphylaxis/sepsis is profound vasodilation because of cytokines and cellular degranulation. This LOW SVR state causes a drop in preload/filling pressure, and leads to a high-output cardiac failure. These are the only shock states with increased cardiac output. A CNS injury causes depression across the board, with low cardiac output, low filling pressures, and low SVR.
Now, there’s good news and bad news. The good news is that examples of shock in USMLE vignettes should be pretty straightforward in suggesting one of the above etiologies.
The bad news is, in real practice, things aren’t so cut and dry. Septic shock and cardiogenic shock have a lot of overlap. Septic shock can cause a septic cardiomyopathy, and cause a decrease in heart function on top of the profound vasodilation, really sending blood pressure down the toilet.
The reverse can also happen. If forward flow is depressed enough, oxygen-starved organs can become ischemic and necrotic, pouring nasty humours (cytokines & bacteria!) into the bloodstream and leading to sepsis atop an already crappy heart.
It will be up to you to put together a story of what’s going on inside your patient, never relying on a singular lab value or test result, and instead, arriving at your conclusion by interpreting all the data that comes your way.