Mastering Mnemonics: SIGECAPS & I CAN’T REST for Depression & Anxiety Screening
- by
- Apr 14, 2021
- Reviewed by: Amy Rontal, MD

Dr. Brian Radvansky and Dr. Taylor Purvis contributed to this post.
SIGECAPS is an incredibly useful screening tool for depression. Given the incredibly high prevalence of depression, you’ll certainly want to keep this mnemonic in your back pocket.
Another mood disorder that you’ll commonly see in the clinic is generalized anxiety disorder, or GAD. It’s helpful to have another short mnemonic in place—I CAN’T REST—in case you think GAD might be at play.
We will begin by breaking down each of these mnemonics and finish with the value add: what we know about exactly how the USMLE tests and how your clinic and hospital patients will present with this diagnosis.
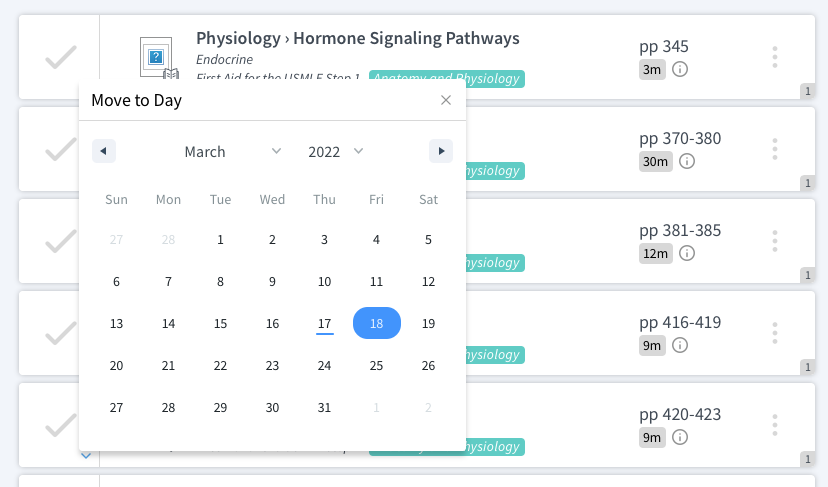
Breaking Down the SIGECAPS Mnemonic for Diagnosing Depression
Sleep changes: Can happen in either direction; either spend all day in bed or anxiety/mania keeping a patient awake. Patients often wake up earlier than desired and cannot fall back to sleep.
Interest (loss of): The question here is, “Do you still find enjoyment in doing the things you like?” When the avid fisherman can’t be bothered to pick up his rod and reel, think of depression. Also known as “anhedonia.”
Guilt: Self-explanatory; blaming oneself for interpersonal or larger problems that are not one’s fault.
Energy: Usually a lack of energy. If the energy cup runneth over, consider mania/bipolar disorder.
Concentration: Loss of some cognitive abilities, like memory and focus.
Appetite: Can swing in either direction, with binge eating or anorexia.
Psychomotor changes: Again, either direction: a general slowing or anxious increase in speed.
Suicidal ideation: A spectrum from self-harm to suicide.
How to Use SIGECAPS for the USMLE and in the Clinic
Now, what can we tell you about how this will present on your exam and with your patients? It will be rare that you will have to count out each and every one of the five out of nine symptoms (score a free point for “depressed mood”).
Your vignette should pitch you a pretty straightforward picture of a depressed patient.
But here’s where they can trip you up. Oftentimes you will have to tease away the diagnosis of “major depressive disorder” from other similar diagnoses.
For instance, if drug intoxication is to blame, then you are likely dealing with substance abuse disorder instead of “major depressive disorder (MDD).”
If the patient is experiencing manic episodes as well, it’s bipolar disorder, and not mere MDD.
If the sadness is in reaction to a major life event, it might be grief/bereavement (loss of spouse), or adjustment disorder (new job in a new city with high levels of stress and anxiety).
Diagnosing Depression in the Elderly Population
Be careful in the elderly population! Many times, depression can present as a form of dementia, sometimes referred to as “pseudo-dementia.” Depression presents differently in everyone, and in the elderly patient population, it can look just like classic cognitive decline.
Make sure your octogenarian’s difficulty concentrating, slow movements, and weight loss can’t be chalked up to a mood change before you label them as having dementia.
Depression Treatments
As far as treatments, the low hanging fruit is the SSRI. These drugs are well-tolerated and almost always are the first-line choice for treatment. Be very familiar with the side effects (e.g., GI upset, sexual dysfunction). Your patient’s best shot at clinical improvement is combining pharmacotherapy with some sort of talk therapy, like cognitive behavioral therapy.
It is your responsibility as a clinician to suss out any suicidal (or homicidal) ideation that your patient might be having, and ensure they are not a danger to him or herself or others.
Since we’re on the topic of mood disorders, let’s focus on another extremely common condition: generalized anxiety disorder (GAD).
Breaking Down the “I CAN’T REST” Mnemonic for Diagnosing Generalized Anxiety Disorder
You can remember the criteria for generalized anxiety disorder (GAD) with the mnemonic “I CAN’T REST.”
Irritability.
Concentration is impaired.
Anxiety, nervousness, worry on most days about many different types of situations, activities, or events.
No control over worry. Debilitating.
Time: at least 6 months.
Restlessness, feeling on edge.
Energy decreased.
Sleep impaired (hard to fall or stay asleep, restless sleep).
Tension in muscles.
To make the formal diagnosis of GAD, you need to have the A, N, and T, plus three or more of the remaining symptoms on more days than not.
So, patients should have excessive anxiety (A) or worry that is difficult to control (N) for at least 6 months (T), with 3 or more of the following additional symptoms: restlessness (R), fatigue (E), difficulty concentrating (C), irritability (I), muscle tension (T), and sleep disturbance (S).
How to Use I CAN’T REST in the Clinic for Patients with Suspected GAD
Remember that making the diagnosis of GAD means another psychiatric illness isn’t responsible for the patient’s symptoms. You’ll also want to exclude any medical conditions or substance use disorder as a potential cause. Common medical conditions that can look like GAD include hyperthyroidism, pheochromocytoma, arrhythmias, and hyperparathyroidism. Substances like albuterol, decongestants, levothyroxine, and caffeine can masquerade as GAD.
GAD Treatments
Like for depression, the first-line therapy is either cognitive-behavioral therapy (CBT) or selective serotonin reuptake inhibitor/serotonin norepinephrine reuptake inhibitor. Choosing between therapy and medication should be based on patient preference and availability—both are great options. Benzodiazepines carry a risk of tolerance and dependence, and are not first-line medications for GAD.
We hope these mnemonics help frame your discussions with patients about their mental health. Keep up the great work!