USMLE Question Breakdown: Cardiac Causes of Syncope
- by
- Dec 03, 2014
- Reviewed by: Amy Rontal, MD
 Syncope is a common topic for a USMLE Step 2 CK question vignette as it has a wide differential diagnosis with endless possibilities for test questions based on pathology, diagnostic workup and management. The question below highlights the reasoning needed to solve a complex three-step question similar in style to the questons you will see on your actual exam.
Syncope is a common topic for a USMLE Step 2 CK question vignette as it has a wide differential diagnosis with endless possibilities for test questions based on pathology, diagnostic workup and management. The question below highlights the reasoning needed to solve a complex three-step question similar in style to the questons you will see on your actual exam.
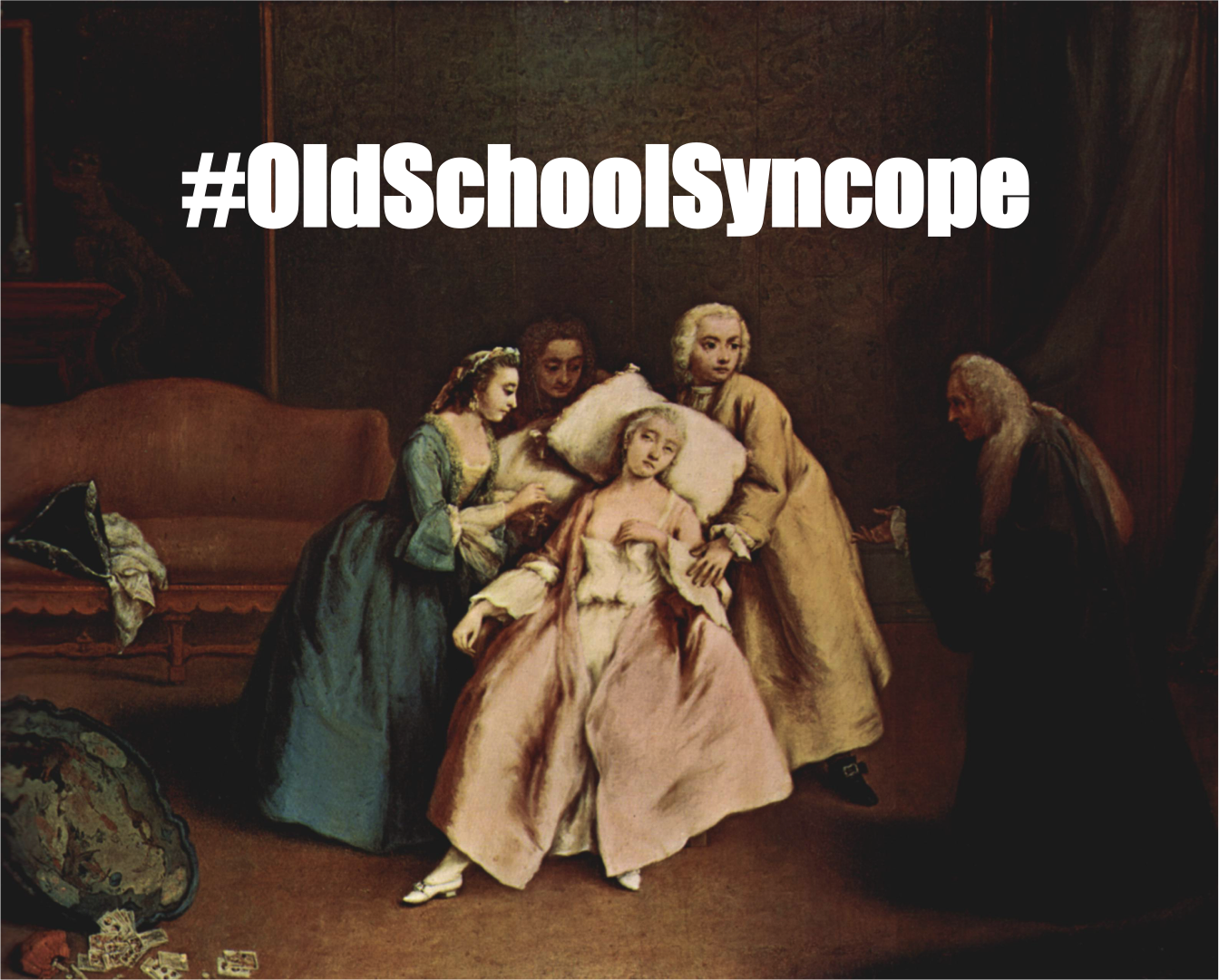
A 28 year old male presents to the ED after a witnessed syncopal event. He was drinking coffee when he noted sudden onset palpitations and dizziness preceding his sudden collapse. The patient regained consciousness after several seconds and did not display any confusion following the event. He denies any bowel or bladder incontinence and observers did not notice any abnormal movements. His past medical history is unremarkable and he is not on any medications. EKG done in the emergency department is shown below:
Which of the following medications would be contraindicated in this patient:
A: Amiodarone
B: Adenosine
C: Procainamide
D: Warfarin
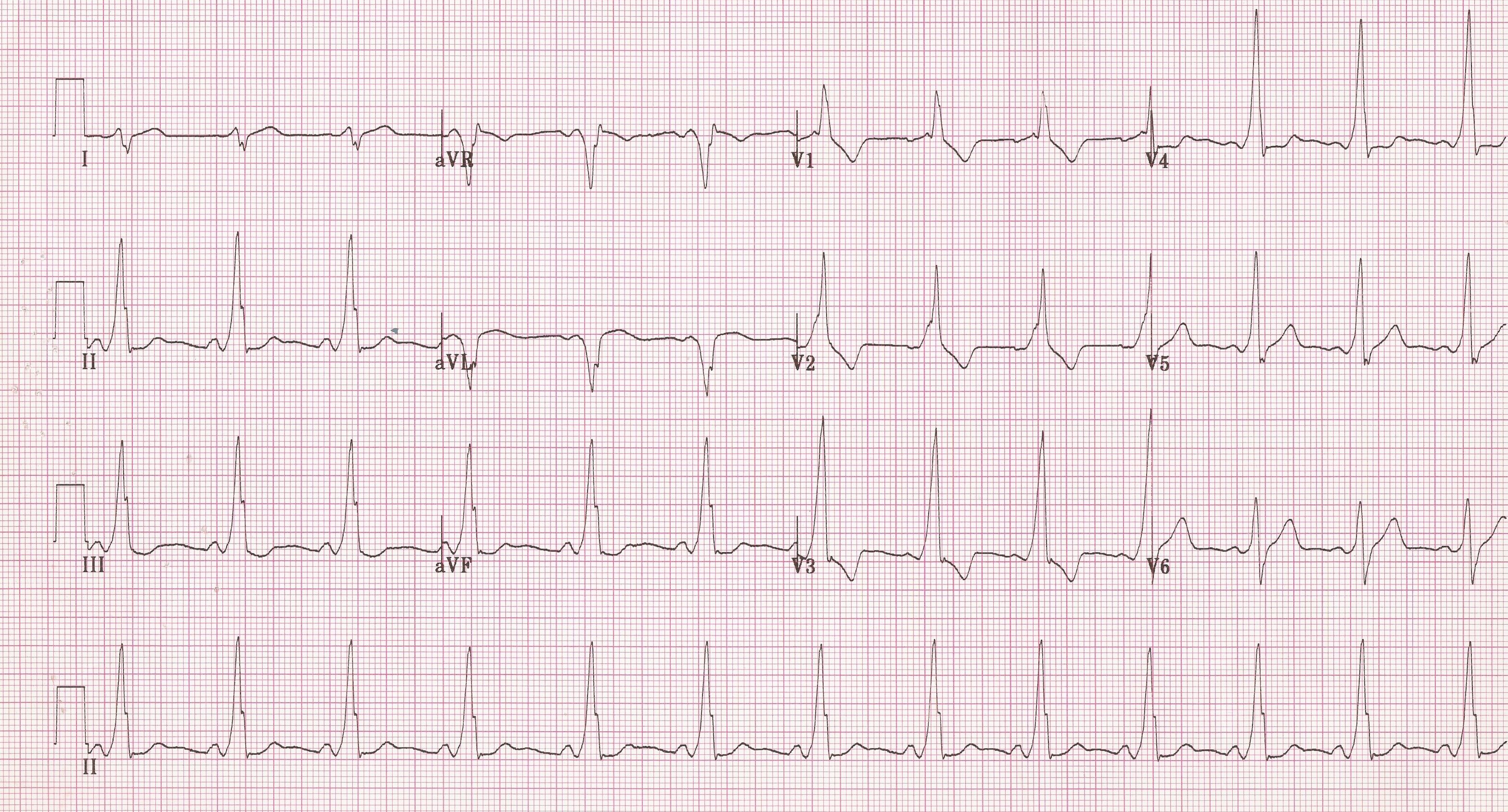
The patient in this question has Wolff Parkinson White, a condition in which an accessory pathway allows for direct electrical communication between the atria and ventricles that bypasses the AV node. As such, drugs like Adenosine that act to slow the AV node are contraindicated because they could worsen symptoms by allowing the accessory pathway to act unopposed.
But let’s break this down further
Again, this is a classic example of a three-step question you will see on the USMLE Step 2 CK.
The first step involves making the correct diagnosis. In this question, we are dealing with syncope in the setting of palpitations, which can have a very wide differential diagnosis. In this question, the diagnosis will be made through correct interpretation of the EKG. Here, note that the patient has a shortened PR interval and a slurred Q wave (delta wave) that is pathognomonic for Wolff Parkinson White.
The second part of this question asks you to identify which medication would be contraindicated in this patient. This requires two separate pieces of knowledge: the pathophysiology of Wolff Parkinson White and the mechanism of action for each drug.
In Wolff Parkinson White, two pathways of conduction exist: the traditional pathway where impulses travel from the SA node through the AV node to the ventricles causing depolarization, and an accessory pathway that bypasses the AV node, directly connecting the atria and ventricles. Impulses traveling down this accessory pathway can cause premature ventricular contractions resulting in a supraventricular tachycardia which can lead to syncope, as seen in this patient.
Finally, let’s look at each medication:
Amiodarone: Prolongs phase 3 of the cardiac action potential
Adenosine: Causes transient block of the AV node
Procainamide: Blocks Na channels to prolong the cardiac action potential and slow conduction
Warfarin: Vitamin K antagonist, anticoagulant
From looking at the answer choices, we can conclude that a drug like adenosine that blocks action at the AV node would lead to unopposed action of the accessory pathway and could worsen symptoms of Wolff Parkinson White. Meanwhile, medications like amiodarone and procainamide that slow conduction by prolonging the action potential could be used to inhibit this accessory pathway. Warfarin would have no role in treating this patient, but it is often used for anticoagulation for patients with atrial fibrillation and atrial flutter.









